Understanding Onycholysis Of The Nail: Causes, Symptoms And Treatment

Onycholysis of the nail is a common nail disorder that occurs when the nail plate separates from the nail bed, resulting in a well-defined area of white opaque nail. This condition can be distressing and cosmetically unacceptable, especially for individuals who work with their hands in public view.
In this comprehensive guide, we will explore the causes, symptoms and treatment options for onycholysis, as well as its potential complications.
What Is Onycholysis Of The Nail?
Onycholysis is a condition characterized by the detachment of the nail plate from the underlying nail bed, it can affect both men and women of all ages and races, but it is most frequently seen in adult women.
Onycholysis can occur in a single nail or multiple fingernails and/or toenails. The distal part of the nail, or the free edge, is commonly affected, causing it to lift and detach. In some cases, the nail may detach laterally or proximally.
Causes of Onycholysis
Onycholysis can be primary, meaning it has an unknown cause, or secondary, resulting from various underlying factors. Some common causes of onycholysis include:
- Trauma: Injury to the nail, such as excessive picking or cleaning under the nail with a file, can lead to onycholysis, this sometimes happen during a pedicure session.
- Skin Diseases: Certain skin conditions, including psoriasis and lichen planus, can cause onycholysis.
- Nail Infections: Fungal infections of the nails, such as those caused by Candida albicans or Pseudomonas aeruginosa, can lead to onycholysis.
- Medications: Some medications, especially those that act as photosensitizers e.g antibiotics including tetracycline, NSAIDs and oral retiniods can cause a specific form of onycholysis known as photo-onycholysis.
- Systemic Events: Onycholysis can be a secondary symptom of systemic conditions like thyroid disorders.
Is Onycholysis Contagious?
It’s important to note that onycholysis caused by injury to the nail, psoriasis, or a reaction to certain medications or nail products is not contagious. However, onycholysis caused by fungal infections can be contagious, primarily through skin-to-skin contact.
Clinical Features Of Onycholysis
The clinical features of onycholysis can vary depending on the underlying cause and severity of the condition. Here are some common signs and symptoms associated with onycholysis:
- Irregular Border: Onycholysis is characterized by an irregular but sharply defined border between the pink portion of the nail and the white edge of the lifted detached nail.
- Nail Appearance: The detached nail is usually white and opaque compared to the transparent normal nail, which appears pink. In some cases, the affected area may have a yellow-pink color.
- Nail Surface: The nail surface may appear normal or exhibit abnormalities such as pitting, indentations, or a crumbly texture.
- Thickened Skin: Hyperkeratotic skin, or thickened skin, may accumulate under the detached nail.
- Subungual Hemorrhage: Acute-onset onycholysis can lead to subungual hemorrhage, characterized by bleeding under the nail.
- Pain: Onycholysis is usually painless, but acute or inflammatory cases can cause discomfort.
It’s important to consult a healthcare professional for an accurate diagnosis and to determine the underlying cause of onycholysis.
Complications of Onycholysis
Onycholysis can predispose the affected nails to secondary infections, most commonly caused by Candida albicans and Pseudomonas aeruginosa, these infections can result in discoloration of the nails.
Additionally, onycholysis can have significant cosmetic implications, particularly for individuals whose hands are frequently visible to the public.
Diagnosing Onycholysis
Onycholysis is primarily diagnosed based on clinical examination and a thorough medical history. In some cases, further investigations may be necessary to identify the underlying cause, these may include:
- Nail Clippings or Scrapings: Samples of the affected nail may be collected for bacterial and/or fungal culture to identify any potential infections.
- Blood Tests: Blood tests, such as thyroid function tests, may be performed to assess for systemic causes of nail disease.
Seeking medical advice is crucial to ensure an accurate diagnosis and appropriate treatment plan.
Differential Diagnosis For Onycholysis
Onycholysis should be distinguished from other nail conditions that may present with similar symptoms. It’s essential to consider the following differential diagnoses:
- Continued Trauma: Persistent nail trauma, such as ongoing nail picking or cleaning, can cause onycholysis to persist or worsen.
- Photosensitizing Drugs: If the onycholysis is caused by the ingestion of photosensitizing medications or substances, discontinuing or changing the offending agent may be necessary.
- Subungual Squamous Cell Carcinoma: In rare cases, onycholysis can be a sign of subungual squamous cell carcinoma, a type of skin cancer.
- Melanoma Of The Nail Unit: Another rare but serious condition that should be considered is melanoma of the nail unit.
Leukonychia, a condition characterized by white discoloration of the nail, including Terry nail, should also be differentiated from onycholysis. Leukonychia refers to a nail that remains attached but appears white and opaque.
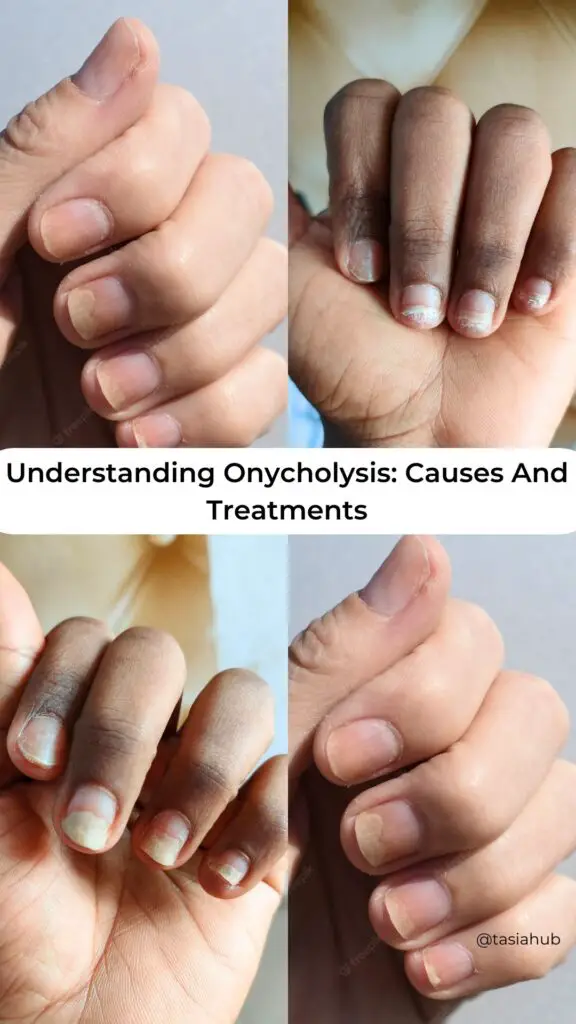
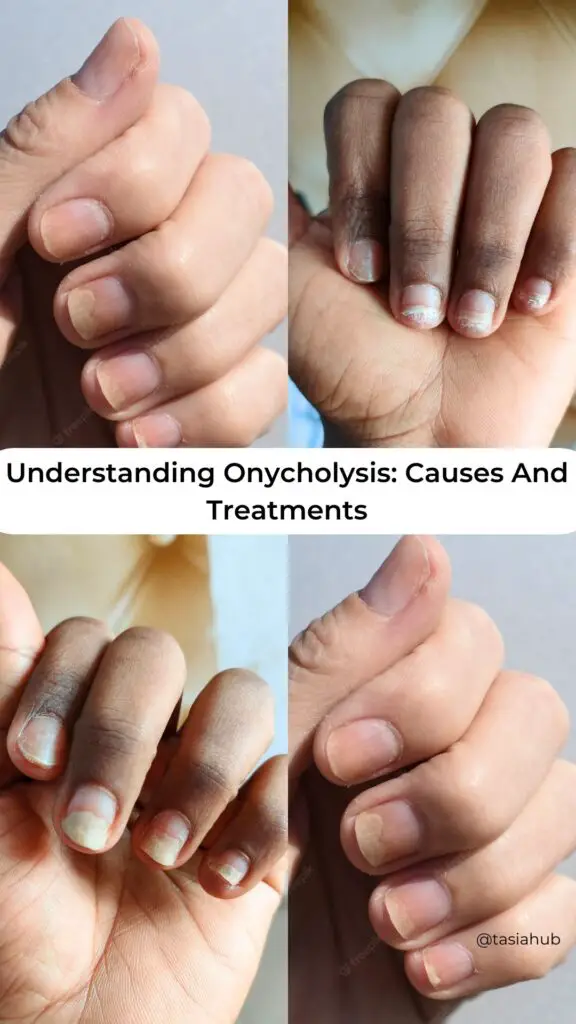
Onycholysis Before And After
I experienced onycholysis, and there were several possible reasons. I’m unsure which one caused it, but it could be due to aggressive filing, using a different glue, or constant tapping on the keyboard.
What I did to regrow my nails:
I regularly kept my nails short, minimized exposure to water, and refrained from using acrylics or any type of coating on my fingers and it took approximately eight months for my nails to fully regrow, as shown in the photos below.




Treatment Options For Onycholysis
The treatment of onycholysis aims to promote the reattachment of the new nail growth to the underlying nail bed, the specific treatment approach will depend on the underlying cause. Here are some general and specific measures that may be employed:
General Measures:
- Nail Trimming: Clipping the affected portion of the nail and keeping the nails short with frequent trimming can help manage onycholysis.
- Minimizing Trauma: Avoiding activities that traumatize the nails and nail beds, such as excessive picking or cleaning, is essential.
- Avoiding Irritants: Minimize exposure to potential irritants like nail enamel, enamel remover, solvents, and detergents.
- Protecting the Nails: Wearing gloves, especially when engaging in wet work, can help protect the nails from further damage.
- Taping the Nail: Taping the detached nail to the underlying digit can provide support and promote reattachment.
- Antimicrobial Soaks: Using antimicrobial soaks, such as dilute vinegar, can help minimize the risk of secondary infections.
Specific Measures:
The specific treatment of onycholysis will depend on the underlying cause, this may involve:
- Medication Adjustment: If the onycholysis is caused by a medication, discontinuing or changing the medication under medical supervision may be necessary.
- Nail Infection Treatment: Treating any underlying fungal or bacterial infections of the nails may help resolve the onycholysis.
- Managing Systemic Conditions: Addressing any systemic conditions, such as thyroid disorders, may help improve nail health and promote reattachment.
It’s important to consult with a healthcare professional or dermatologist for an accurate diagnosis and personalized treatment plan.
Outlook for Onycholysis
The outlook for onycholysis depends on the underlying cause and the duration of the condition. Onycholysis of short duration and known origin has a good prognosis with appropriate treatment.
Fingernails typically take 4-6 months to fully regrow, while toenails may take twice as long, it’s important to note that the longer onycholysis persists, the less likely new nail growth will reattach due to potential permanent damage to the underlying nail bed.
Will Onycholysis Go Away On Its Own?
Yes, onycholysis can go away on its own if you can trim down the fingernails every time it grows out, avoid soaking your hands in water, and avoid acrylics for the next 6 -10 months depending on how fast your healing process is.
How Long Does Onycholysis Take To Heal?
Onycholysis takes anywhere from 6 – 8 months to heal completely, this though is not a guaranteed number if your nail growing process is slow and you fail to follow the steps above.
Is Onycholysis Permanent?
No, onycholysis is not permanent but can reoccur several times if the causes are not addressed.
What Deficiency Causes Onycholysis?
Iron Deficiency
Iron deficiency refers to a condition where the body lacks a sufficient amount of iron, an essential mineral for various bodily functions. Iron plays a crucial role in the formation of hemoglobin, a protein in red blood cells that carries oxygen from the lungs to the rest of the body. When the body doesn’t have enough iron, it can lead to a reduction in the production of red blood cells, resulting in a condition known as iron deficiency anemia.
Common symptoms of iron deficiency may include fatigue, weakness, pale skin, shortness of breath, cold hands and feet, dizziness, and headaches. In addition to anemia, iron deficiency can impact overall health and cognitive function.
Iron deficiency can occur due to various reasons, including inadequate dietary intake of iron, poor absorption of iron from the diet, increased demand during growth or pregnancy, and chronic blood loss from conditions like gastrointestinal bleeding or menstruation.
Treatment often involves iron supplementation and addressing the underlying cause of the deficiency. It’s important for individuals experiencing symptoms of iron deficiency to consult with a healthcare professional for proper diagnosis and management.
Conclusion
In conclusion, onycholysis is a nail disorder characterized by the detachment of the nail plate from the nail bed. It can have various causes, including trauma, skin diseases, nail infections, medications, and systemic events.
Onycholysis can be diagnosed at home or through clinical examination and, if necessary, further investigations. The treatment approach will depend on the underlying cause and may involve general measures such as nail trimming and minimizing trauma, as well as specific measures such as medication adjustment or treating nail infections.
Seeking medical advice is crucial for an accurate diagnosis and appropriate management of onycholysis.